Accusations of financial malfeasance related to coronavirus testing have been the subject of numerous news stories. The alleged abuses include overcharging for coronavirus testing both nationally and internationally (1, 2, 3), and loopholes in U.S. federal law allowing patients to be charged when the law’s intention is complete financial coverage (4). In the U.S., problematic medical fees and billing practices are not restricted to coronavirus testing: They are commonplace throughout the healthcare system.
In a previous article, we described lab stewardship as a set of activities, policies, and procedures that improve five elements of lab testing: access to testing, test ordering, result retrieval, result interpretation, and financial
fairness for patients (5). We also explained why lab stewardship must be patient-centered. Here we describe how laboratories can help patients with financial decisions and avoid subjecting them to financial toxicity.
The concept of financial toxicity in medicine was first described in oncology, where patients disproportionately experience financial harm from their care (6, 7). Financial toxicity both hurts the patient financially and harms the patient’s health due to stress and the avoidance of necessary care (8). Table 1 presents financial fairness goals for lab stewardship programs and builds on the work of Elizabeth Rosenthal, MD, who has advocated for a patient financial bill of rights (9).
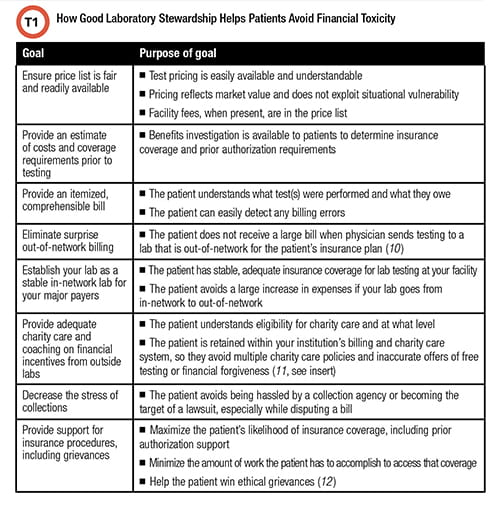
See Table 1 in CLN October PDF
Pricing and Financial Toxicity
The list price of laboratory testing is highly variable. It is not uncommon to see list prices substantially above costs. These high fees can result in financial toxicity to patients, especially if patients are uninsured or underinsured, or if testing is out of network for the patient’s health plan (13). Hospitals sometimes raise prices in order to increase revenue from the subset of uninsured patients who have the ability to pay, as well as insured patients who have to pay out-of-pocket when testing is not covered by their health plan or is out-of-network. High prices also lead to higher reimbursement when insurance plans are contracted to pay hospitals a percentage of billed charges. Hospitals’ justifications for high prices usually focus on the availability of charity care, and the fair prices available to patients who are insured and in-network.
While clinical laboratory leaders rarely determine the pricing for lab tests, that need not prevent them from influencing pricing behavior. Clinical laboratory leaders practice patient-centered stewardship when they involve themselves in health system finances to advocate for fair pricing. Reasonable pricing directly decreases financial toxicity.
Price Transparency and Out-of-Pocket Expenses
Most commercially insured patients cannot rapidly determine out-of-pocket expenses for lab testing because price lists are confusing and difficult to access. Many hospital websites do not provide easy calculation of out-of-pocket expense based on insurance plan (or lack thereof), let alone communicate eligibility for charity care. Thus, healthcare remains one of the few purchased services where a person does not know the estimated payment before a service is rendered.
Fortunately, some hopeful examples of better pricing and estimating practices have appeared. For example, the website for Prevention Genetics provides a well-formatted, accurate price list of their tests and test panels (14). The state of New Hampshire provides a price transparency tool that provides patients with estimated test costs at different hospital and commercial labs based on the patient’s insurance plan (15).
Improving Insurance Coverage
A patient-centered lab stewardship program has numerous ways to help patients obtain better coverage for medically necessary testing. For example, laboratory experts, including lab genetic counselors, can guide providers to write medical notes that support the necessity of testing, emphasizing how the test influences medical care. The medical documentation should align with plan-specific coverage criteria.
Another way labs can help patients is to regularly meet with commercial and government payers to provide updates on medical necessity. For example, Seattle Children’s, as well as other labs in the PLUGS collaboration, have successfully worked with commercial payers and state Medicaid systems to improve coverage for genetic testing. These interactions with payers build trust, which has the added benefit of increasing the likelihood that your lab will remain in-network for the patient’s insurance.
Lab experts also can support appropriate grievances, in which the patient disputes a noncoverage decision. Some insurance plans will allow patients to give the lab permission to appeal on behalf of the patient. When that is not possible, labs still can provide guidance and tools. For example, the PLUGS collaboration has produced a free tool to help patients win ethical grievances for coverage of their laboratory tests (12).
When Laboratories Put Patients First, It Makes a Difference in Their Care
Clinical laboratories practice patient-centered laboratory stewardship when they decrease the financial toxicity of testing. Clinical laboratories can pursue a variety of goals to prevent financial toxicity and increase financial fairness. When patients are treated fairly by laboratories, they are more likely to obtain and benefit from medically recommended testing.
Michael Astion, MD, PhD, is clinical professor of laboratory medicine at the University of Washington department of laboratory medicine, and medical director of the department of laboratories at Seattle Children’s Hospital. + EMAIL: [email protected]
Brian R. Jackson, MD, is associate professor at the University of Utah School of Medicine and medical director of support services, IT and business development at ARUP Laboratories in Salt Lake City. +EMAIL: [email protected]
References
- Vaidya A. BCBS of Kansas City sues Covid-19 testing provider over alleged price gouging. MedCity News. July 26, 2021. https://medcitynews.com/2021/07/bcbs-of-kansas-city-sues-covid-19-testing-provider-over-alleged-price-gouging/ (Accessed August 24, 2021).
- Kliff S. It felt like deception: an elite NYC hospital charges huge virus test fees. New York Times. March 30, 2021. www.nytimes.com/2021/03/30/upshot/covid-test-fees-lenox-hill.html (Accessed August 24, 2021).
- Browning S. Covid testing is ripoff, says former regulator. BBC News. August 17, 2021. https://www.bbc.com/news/business-58200203 (Accessed August 23, 2021).
- Lazarus D. Coronavirus tests are supposed to be free. But there’s a nasty loophole in the lab. Los Angeles Times. August 19, 2021. www.latimes.com/business/story/2021-08-19/column-covid-tests (Accessed August 24, 2021).
- Astion M and Jackson BR. 2021. Moving Toward Patient-Centered Laboratory Stewardship. Clinical Laboratory News 2021;47(7):32-33.
- Goozner M. Editorial: An epidemic of financial toxicity. Modern Healthcare. August 30, 2019. https://www.modernhealthcare.com/opinion-editorial/editorial-epidemic-financial-toxicity (Accessed July 27, 2021).
- National Cancer Institute. Financial Toxicity (Financial Distress) and Cancer Treatment. https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-pdq (Accessed August 24, 2021).
- National Cancer Institute. National Cancer Institute Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/financial-toxicity (Accessed July 21, 2021).
- Rosenthal E. Nine Rights Every Patient Should Demand: We need a Financial Bill of Rights to protect consumers of health care from unfair charges. New York Times. April 27, 2018. www.nytimes.com/2018/04/27/opinion/sunday/patients-rights-hospitals-health-care.html (Accessed August 24, 2021).
- Knauss K. Out of Network Lab Costs Can Be Expensive. https://insuremekevin.com/out-of-network-lab-costs-can-be-expensive/ (Accessed July 22, 2021).
- Astion M. Convincing providers and patients to keep testing within your hospital and laboratory’s utilization management system. Clinical Laboratory News 2017;43(4):24-25.
- Seattle Children’s Patient-centered Laboratory Utilization Guidance Services. Patient Toolkit for Complex Lab Tests: How to get them Covered. https://www.schplugs.org/plugs-patient-toolkit/ (Accessed July 29, 2021).
- Evans M, Mathews AW, McGinty T. Hospitals often charge uninsured people the highest prices, new data show. Wall Street Journal. July 6, 2021. www.wsj.com/articles/hospitals-often-charge-uninsured-people-the-highest-prices-new-data-show-11625584448 (Accessed August 23, 2021).
- Prevention Genetics Testing. https://www.preventiongenetics.com/searchTests?val=all+tests&filter=num (Accessed July 27, 2021).
- New Hampshire Insurance Department. NH Health Cost. https://nhhealthcost.nh.gov/costs/select (Accessed July 27, 2021).
- Rogers BB, Adams JL, Carter AB, et al. The impact of disruption of the care delivery system by commercial laboratory testing in a children’s health care system. Arch Pathol Lab Med 2019;143(1):115-121.

