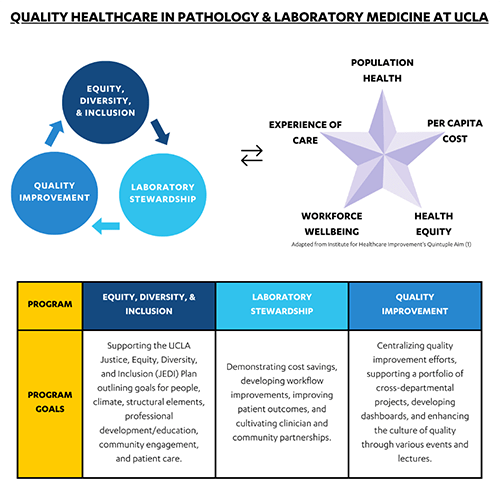
Our Department of Pathology & Laboratory Medicine at the University of California, Los Angeles (UCLA) is committed to optimizing patient outcomes. In support of this mission, our department has invested in several programs to enhance our clinical services: quality improvement (QI), laboratory stewardship (LS), and equity, diversity, and inclusion (EDI). Although each program has its own distinct initiatives, they each share the overarching goals of the quintuple aim for healthcare improvement: 1) improving population health, 2) enhancing the care experience, 3) reducing costs, 4) addressing clinician burnout, and 5) advancing health equity (Figure 1) (1).
To optimally align our QI, LS, and EDI activities, and to promote collaboration among them, our department hired a program manager to support all three programs. A program manager is a strategic project-management professional who oversees and coordinates projects and strategic initiatives across an organization or department. This article illustrates how clinical laboratories and health systems can incorporate program managers to promote collaboration, innovation, and patient-centered healthcare.
What background and education does a program manager typically have?
Program managers in healthcare can have a variety of backgrounds and typically have both an undergraduate and master’s degree. Our program manager, Monique, obtained a bachelor’s degree in environmental science before beginning her healthcare career with patient-facing roles as a medical assistant and receptionist. She then obtained a certificate in accounting and moved up the ranks in clinical finance positions at UCLA, first in obstetrics & gynecology and then in pediatrics. These roles equipped her with a deep understanding of the operations of an academic medical center and fueled her passion for enhancing systems and processes. She then transitioned to her current role as a program manager for pathology & laboratory medicine as she was one year into a two-year Master of Healthcare Administration program in health policy and management.
Although academic qualifications are essential, Monique’s success also hinges on her mastery of soft skills such as leadership, communication, and problem-solving. These abilities enable her to effectively navigate the complex landscape of healthcare program management, fostering collaboration and driving innovation across QI, LS, and EDI initiatives.
What does a day in the life of a program manager look like?
As a program manager supporting QI, LS and EDI, Monique oversees various strategic initiatives and projects focused on continuous quality improvement, value-based healthcare, and advancing health equity. Each program has its own committees and dedicated faculty and staff cochairs, with whom Monique works closely. Supporting these programs and their numerous individual projects and priorities requires strong organizational skills, attention to detail, and a collaborative approach.
Each day requires her to wear a different hat depending on the task at hand. Monique’s previous experiences equipped her with a diverse skill set, allowing her to serve as a strategist, marketer, project manager, finance analyst, data analyst, programmer, or operations analyst. On any given day, Monique may:
- Lead meetings (scheduling, agendas, meeting minutes, action items)
- Develop strategies and manage project plans (Reports to define project backgrounds, problem statements, proposed actions, data metrics)
- Support laboratory personnel in retrieving and analyzing data (laboratory, clinical, financial) and developing dashboards
- Create visual content to share project status updates and successes, or to promote relevant events (slide decks, website design, posters, flyers)
How can a common program manager for QI, LS, and EDI align these priority areas?
The alignment of the QI, LS, and EDI programs has strengthened collaborations both within and outside of our department. For the LS program, expertise and advice from the QI group have allowed us to optimize the approach and structure of our stewardship initiatives.
Collaboration with the EDI group has empowered us to promote equity, diversity, and inclusion both in how we structure stewardship project groups and in how we take a patient-centered approach when designing stewardship interventions. As an example, one of our most successful stewardship initiatives to date focuses on reference laboratory test utilization. Monique organized and delegated a review by faculty subject matter experts of tests historically sent through “miscellaneous” (nondiscrete) test orders in the electronic health record (EHR) to evaluate test appropriateness and to select the most optimal tests and reference labs. We then built 45 (and counting) new discrete tests into the EHR, and Monique designed an automated email tool to send targeted provider notifications about the newly built tests. Through this project, we have been standardizing our reference lab test offerings across our health system and improving access to the most appropriate, high-quality, and cost-effective tests, regardless of the patient’s location.
How can institutions justify program managers for these areas?
It’s important to acknowledge potential challenges to hiring program managers. These might include concerns about resource allocation or the perceived need for additional layers of management. However, we believe that by demonstrating the tangible benefits and return on investment associated with program managers, coupled with effective communication of their role in driving organizational success, these concerns can be addressed effectively.
Our QI, LS, and EDI programs have been successful due to the extraordinary support of our department chair, dedicated faculty and staff cochairs, and high-level visibility across our health system. For LS, in addition to a department-driven laboratory stewardship committee, we have a Laboratory Stewardship Oversight Committee (LSOC) composed of key health system leaders (2). Monique leads a quarterly LSOC meeting in which we share with these leaders our latest stewardship successes and challenges and seek feedback about active areas of priority for the health system. Quantifying and sharing successes in this way has led us to continuously iterate and expand our initiatives with support from the highest levels.
Our QI, LS, and EDI programs have each developed so successfully over the past few years that we recently hired a second program manager to support them. With our program management capacities now increased, we are seeking to expand our efforts to incorporate trainee education and involvement in projects and to share our successes externally via conference abstracts and publications. Further, we are integrating our program managers into our Laboratory Medicine Informatics division to optimally incorporate data analytics and clinical decision support design, etc. to support our LS initiatives. Overall, our program managers will ensure strategic alignment, cross-functional coordination, and outcomes realization in support of our missions of improving patient and population health.
Acknowledgements
The authors gratefully acknowledge Maria Estrada, MHA, PMP, our recently-hired second program manager, for reviewing this article.
Monique Trinh, MHA, is a program manager in the department of pathology and laboratory medicine at the David Geffen School of Medicine, University of California at Los Angeles in California. +Email: [email protected]
Allison Chambliss, PhD, DABCC, FADLM is an associate clinical professor in the department of pathology and laboratory medicine at the David Geffen School of Medicine, University of California at Los Angeles in California.
References
1. Nundy S, Cooper LA, Mate KS. The quintuple aim for health care improvement: A new imperative to advance health equity. JAMA. 2022;327(6):521-522.
2. Dickerson JA, Fletcher AH, Procop G, Keren DF, Singh IR, Garcia JJ, Carpenter RB, Miles J, Jackson B, Astion ML. Transforming laboratory utilization review into laboratory stewardship: Guidelines by the PLUGS National Committee for Laboratory Stewardship. J Appl Lab Med. 2017 doi: 10.1373/jalm.2017.023606.
