Summary
DOI: 10.1373/clinchem.2016.263756
A 32-year-old man presented with severe abdominal pain and ascites. His medical history included diagnosis of Sandifer syndrome, scoliosis requiring 3 spinal surgeries, microgastria, and hiatal hernia repair, and most recently, laparoscopic cholecystectomy (7 weeks prior).
Student Discussion
Student Discussion Document (pdf)
Lusia Sepiashvili,1 Ashley R. Dahl,2 Jeffrey W. Meeusen,1 Conor G. Loftus,2 and Leslie J. Donato1*
1Department of Laboratory Medicine and Pathology, 2Department of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN.
*Address correspondence to this author at: Department of Laboratory Medicine and Pathology, Mayo Clinic, Hilton 3-10B 200 First St. SW, Rochester, MN, 55905. Fax 507-266-4088; e-mail [email protected]
Case Description
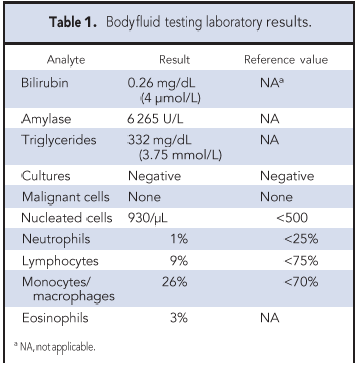
A 32-year-old man presented with severe abdominal pain and ascites. His medical history included diagnosis of Sandifer syndrome, scoliosis requiring 3 spinal surgeries, microgastria, and hiatal hernia repair, and most recently, laparoscopic cholecystectomy (7 weeks prior). Postprocedural abdominal pain led to a computed tomography (CT)3 scan which confirmed ascites. The possibility of a postcholecystectomy common bile duct leak prompted an endoscopic retrograde cholangiopancreatography (ERCP) with stent placement. Unfortunately, this did not prevent peritoneal fluid from reaccumulating and the patient was transferred to our institution for further evaluation and management. The patient was afebrile and vital signs were normal. The abdominal examination revealed mild diffuse nonspecific tenderness. CT scan of abdomen was performed revealing increased peritoneal fluid. The radiologist noted that the findings were likely iatrogenic and could represent a bile, lymph, or pancreatic leak. CT guided paracentesis aspirated 280 mL of fluid accumulated near the right hepatic lobe and paracolic gutter. Aspirate was described as watery opaque and white with a pink tinge. Results of body fluid laboratory analyses are described in Table 1.
Questions to Consider
- What is the utility of body fluid lipid analysis in the differential analysis of a body fluid specimen?
- How is definitive diagnosis of a chyle leak achieved?
- What is the potential benefit of lipoprotein electrophoresis analysis on fractions of an ultracentrifuged body fluid as compared to the whole fluid?
- What is the concern with using a triglyceride assay that does not blank for endogenous glycerol?
Final Publication and Comments
The final published version with discussion and comments from the experts appears in the July 2017 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case Study for personal or classroom discussion use. When photocopying, please make sure the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2016.263756
Copyright © 2017 American Association for Clinical Chemistry
